If someone is in crisis (distressed, disoriented, or at risk) what you do next matters.
You're not expected to be a therapist. Or a hero. Or the Dalai Lama with a 9-iron.
But you can make a difference by knowing what to look for, what to say, and how to stay steady when things feel scary.
This guide will walk you through how.
Quick takeaways
Critical situations need clear action:
- Trust your instincts. If something feels seriously wrong, it probably is.
- Stay calm and present. Your steadiness helps them feel safer.
- Ask directly. "Are you thinking about suicide?" won't put the idea in their head.
- Don't leave them alone if you're worried about immediate safety.
- Call for help. Emergency services (999/911), or take them to A&E / the ER.
- Listen without trying to fix. Sometimes just being heard is what keeps someone going.
- Follow up. Check in again tomorrow, next week. Your ongoing presence matters.
What Is a Mental Health Crisis?
A mental health crisis is when someone’s struggling to cope, stay safe, or function, and it’s reached a breaking point.
That might look loud. Or quiet.
Clear as day. Or hard to pin down.
It might look like risky behaviour or complete withdrawal. Panic, confusion, or hopelessness. Talking about ending things. Or simply struggling to hold it together.
What matters is that someone isn’t okay in this moment, and they may need urgent help to stay safe physically, mentally, or emotionally.
You don’t have to diagnose or know the full story.
You just need to notice when something feels off, and respond with calm, clear steps.
{{divider-main="/content-templates"}}
What Crisis Can Look Like
Crisis can show up in many ways: sometimes dramatic, sometimes subtle.
Direct statements:
- "I don't want to be here anymore"
- "People would be better off without me"
- "I can't take this anymore"
- "I just want it to stop"
- "There's no point"
Behavioural changes:
- Completely shut down (blank, frozen, or numb)
- Panicked, overwhelmed, or struggling to speak clearly
- Acting recklessly or putting themselves in danger
- Behaving in ways that seem completely out of character
- Giving away possessions or "getting affairs in order"
- Sudden calmness after a period of distress (can indicate they've made a plan)
Emotional signs:
- Talking about feeling trapped, hopeless, or not seeing a way out
- Extreme mood swings or emotional numbness
- Expressing intense shame, guilt, or feeling like a burden
- Talking about unbearable pain (emotional, not physical)
You might not know exactly what's going on. That's okay. What matters is noticing when something feels serious and staying with it long enough to help them get the support they need.
{{divider-main="/content-templates"}}
What You Can Do in the Moment
When someone is in crisis (panicked, withdrawn, or saying things that scare you) it’s hard to know what to do. You might freeze. You might worry about saying the wrong thing. You might want to run for a grown-up, only to realise… you are the grown-up.
This section gives you a steady path forward using ALGEE, a proven approach from Mental Health First Aid. It's used by trained responders, but it works just as well for anyone who cares enough to show up.
Here’s more information about ALGEE by Mental Health First Aid.
It will help you stay calm, make sense of what’s happening, and guide someone toward the support they need.
A — Approach and assess for risk of harm
Step in. Quietly. Calmly.
If you think someone might be in crisis, don’t wait for the perfect words. You can start with:
“Hey. I’m not sure you’re okay right now, and I want to check in.”
Be direct. If they say something worrying (like wanting to disappear, feeling hopeless, or planning to hurt themselves) it’s okay to ask:
“Are you thinking about suicide?”
You won’t put the idea in their head. You’re just naming something they might be too scared to say. And that alone can be life-saving.
If someone is at immediate risk (talking about ending their life, acting recklessly, or unable to keep themselves safe) call 999 (UK) immediately. Stay with them if you can.
L — Listen non-judgementally
This part matters more than you think.
You don't need the right advice. You just need to be there. Stay present. Don't interrupt. Let silence happen. Let anger happen. Let tears happen.
Use simple, open prompts:
- "What's going on for you right now?"
- "I'm here. You don't have to hold it alone."
- "Tell me more about that."
Avoid these common mistakes:
- "Everything happens for a reason"
- "Things could be worse"
- "You have so much to live for"
- "Just think positive"
Judgment, even the helpful kind, can shut people down fast. You're not here to analyse or fix. Just listen.
G — Give reassurance and information
When someone's in crisis, the world can feel warped. Their thoughts might be racing, looping, or completely blank.
You can steady the moment by offering calm, grounded reassurance:
- "You're not on your own in this."
- "There is help for what you're feeling."
- "You don't have to figure this out alone."
Don't sugar-coat or overpromise. Keep it honest. Keep it human.
You can also gently name support options like their GP, Samaritans (116 123), NHS 111, or local mental health services.
E — Encourage professional support
Once things feel a bit more stable, encourage them to take a next step, however small:
- "Would you feel okay calling your GP or doctor?"
- "Want me to sit with you while you call a support service?"
- "We could go together if that makes it easier."
It might take time. They might say no. That's okay. You've planted a seed and shown them it's worth acting on.
E — Encourage self-help and other supports
You can also point them toward things that have helped them in the past, if you know what those are. A trusted person. A calm place. A familiar routine.
If they're open to it, help them make a short plan: Who could they call tonight? What's one thing that might help them feel even a bit safer or steadier?
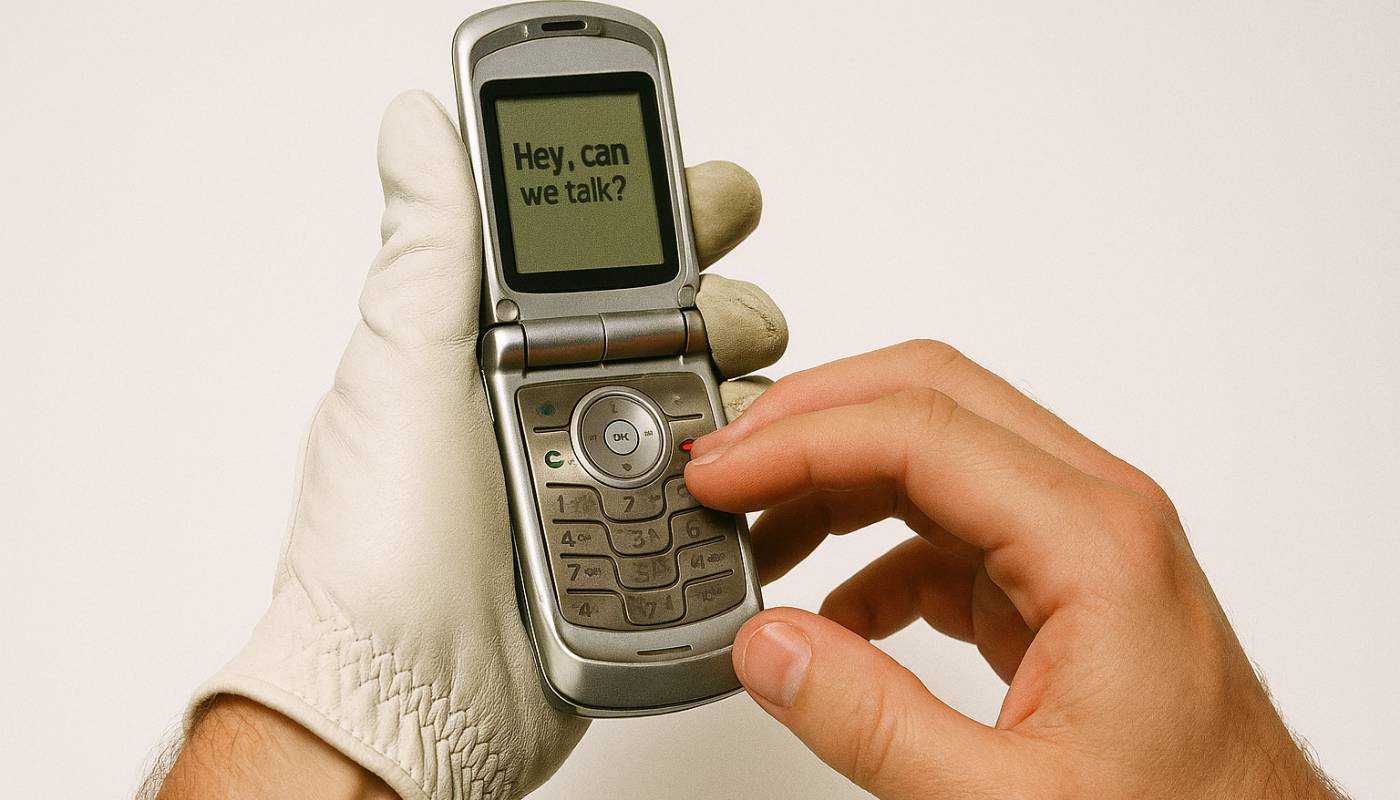
And let them know you'll check in again. Tomorrow. Next week. Quietly keeping someone tethered can be more powerful than it looks.
{{divider-main="/content-templates"}}
If Someone Is Suicidal or in Immediate Danger
If someone tells you they’re feeling suicidal, hopeless, or like they can’t go on, take it seriously.
You don’t need to say the perfect thing. Just stay calm, be present, and help them get support.
Call Emergency Services
If someone is at serious risk and needs urgent help, call the emergency number for your country straight away. Tell them clearly that you’re with someone who is at risk of suicide or severe mental distress. They’ll guide you on what to do next.
Stay With Them
Don't leave them alone unless you absolutely have to. Just being there, quietly and patiently, can help keep them tethered. You don't need to talk much. You just need to stay.
Get Them to Safety
If they're not safe where they are, help them move somewhere calmer or better supported (GP surgery, hospital, trusted friend's home). If you're not sure, aim for A&E or a walk-in crisis centre.
Remove Means of Harm
If it's safe to do so, remove or secure anything they could use to hurt themselves. Don't put yourself in danger, but reduce immediate risks where possible.
{{divider-main="/content-templates"}}
Helpful Contacts and Crisis Support
If someone’s in crisis (or if you are) there are trusted places to turn. They’re confidential, free to use, and run by real humans trained to help in tough moments.
Visit our GET HELP page to learn more.
{{divider-main="/content-templates"}}
After the Crisis
The immediate storm may pass, but what happens next matters too.
Follow up regularly.
Check in tomorrow, next week. A simple "thinking of you, how are you doing?" can make a huge difference.
Don't disappear.
Many people worry they'll be judged or become a burden after opening up about crisis. Showing up consistently proves they matter.
Encourage ongoing support.
Crisis often reveals underlying issues that need professional attention. Gently encourage therapy, GP visits, or mental health services.
Look after yourself too.
Supporting someone through crisis is emotionally demanding. Make sure you have support and take breaks when you need them.
Know your limits.
You're a friend, not a therapist. It's okay to say "I care about you, and I think you need professional help that I can't provide."
If you have concerns about your mental health or well-being, please speak to a qualified health or mental health professional.
%20(13).avif)


.jpg)



.jpg)





.avif)